 Just when you think you could not get any busier…..You get the page….it is a transfer from med surg. Now you know that the transfer is going to suck up all your time because the policy is…
Just when you think you could not get any busier…..You get the page….it is a transfer from med surg. Now you know that the transfer is going to suck up all your time because the policy is…
- The RN from telemetry has to go and pick the patient up and transport the patient to telemetry due to it being a higher level of care.
- The patient has to be transported with a Life Pak /Defibrillator in case something should happen along the road to telemetry.
- The RN from med surg is supposed to accompany the telemetry RN and use their bed or stretcher and the med surg floors Life Pak(They only have ONE Life PAk for the whole floor so how can anyone in good consious take their only Defibrillator? What if they have a code while you are traipse off with their only Defibrillator?).
Now of course number 3 never happens.
What happened is as follows. I go get my own stretcher, I grab my own Life Pak, I beg an escort to come with me. I get to the medical floor. The med surg RN is sitting at a computer charting. I get to the room, the patient has no idea he is being moved, wants to know why he needs that big scary Life Pak, and nothing is packed up.
The med surg nurse jumps up from the computer, starts packing up the patient and I am trying not to snarl at her for giving me the shaft.
This is the same nurse who called to supervisor because I did not call her back fast enough and the patient is not even ready. Yup she gave me the shaft.
Here is the best part of this whole story….
The patient was on a telemetry monitor for stroke protocol due to the patient having a possible TIA. Stoke was already ruled out.
The patient moved…..and the med surg RN decided that the artifact on the telemetry strip was V tach….
So without inquiring expert opinions from another nurse with more experience in interpreting rhythm strips or a physician, the med surg nurse calls the attending who by the way was a nephrologist, and she tells him that that patient had 7 beats of V tach. The attending then orders the patient to transfer to telemetry and a cardiologist consult.
I mean give me a break!
I did all this work, moved the patient why the med surg sat upstairs on med surg on her hind end charting at the computer.
I get the patient on telemetry, got 12 leads, serum chemsitry levels including mg++…and then guess what….???
I look at the alleged 7 beats V tach and find that it was ARTIFACT! Not even close to V Tach, narrow complexes very close together and only in 1 lead!
This is Artifact above us
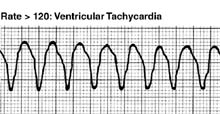
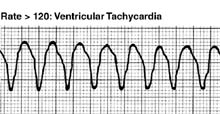
So the above is Ventricular Tachyacardia. Image from AcuteResponse.
Not only did the patient not have any “run of V tach” the patient did not have any ectopy at all. So I am asking the med surg nurse…”Did he have PVCs? Did the patient have any labs this morning? Was the patient symptomatic after this (supposed run of v tach? Did you get a 12 lead EKG? Did you have the house MD see the strip?” No. No. No. No. No.
So I find this unbelievable that this is even permitted!
Then I get the call hours later from ultrasound…the patient was due to have carotid ultrasound and a transcranial doppler as part of the neurological workup and guess what? NO TESTS were done because the med surg nurse informed ultrasound dept, “The patient is to unstable and might “code” at any minute” and therefore could not go to and fro testing.
The worst part was when the med surg nurse said, “You sound irritated (well…duh, I am busy and you called the nursing supervisor because I did not run right up and take the patient off your floor.) I do not know why your so irritated, this is a really nice patient, it is not like you have tons of work to do for him, he is not complete care, not confused.”
WHAT??? “Working” for my patients is what I LOVE to do. Adding a patient to our census that does not need to be here is just one more patient in the ED that with severe CHF or a new onset of rapid atrial fibrillation or NSTEMI that will have to sit in the ED holding area waiting for a bed on telemetry, so that I can do nothing for the ruled out stroke, neurologically intact, “nice” patient who will have his testing done tomorow due to the unstable status of fake V tach as determined by med surg RN, who also might code at any minute. errrr.
Yeah Medical/Surgical Floor transfers to telemetry….love them every time. Usually the patient is totally benign on assessement or a totally septic patient tanking and needing to really go to ICU.
Tags: Defibrillator, Medical Surgical Nurse, patient transfers, Telemetry, Ventriular Tachycardia
 HA!!!
HA!!! Just when you think you could not get any busier…..You get the page….it is a transfer from med surg. Now you know that the transfer is going to suck up all your time because the policy is…
Just when you think you could not get any busier…..You get the page….it is a transfer from med surg. Now you know that the transfer is going to suck up all your time because the policy is…